By Yurlene S. Dela Cruz
I had the privilege to be a Project Creator of a Black Belt Process Improvement initiative on “Crisis Communication.” As a Lean Leader, I focused from a strategic perspective supporting the values of the High Reliability Organization (HRO). Clearly and consistently communicating the “True North” purpose was the most rewarding part of this initiative.
Code Green is the activation of emergency assistance during a disruptive behavior. The Code Green Team includes Mental Health RNs, Psychiatry Providers/Residents, and VA Police. Our Code Green activations have increased during fiscal years 2021 to 2023. Our facility’s Workplace Behavior Risk Assessment (WBRA) further confirmed the increasing trend of disruptive behaviors. They vary from verbal outbursts, physical threats, and physical assaults. The top 5 workplace areas included: 2 Community-Based Outpatient Clinics (CBOC), inpatient medical-surgical units, Community Living Center (CLC), and Emergency Department (E.D.). The process improvement stakeholders excluded CBOCs.
Current State
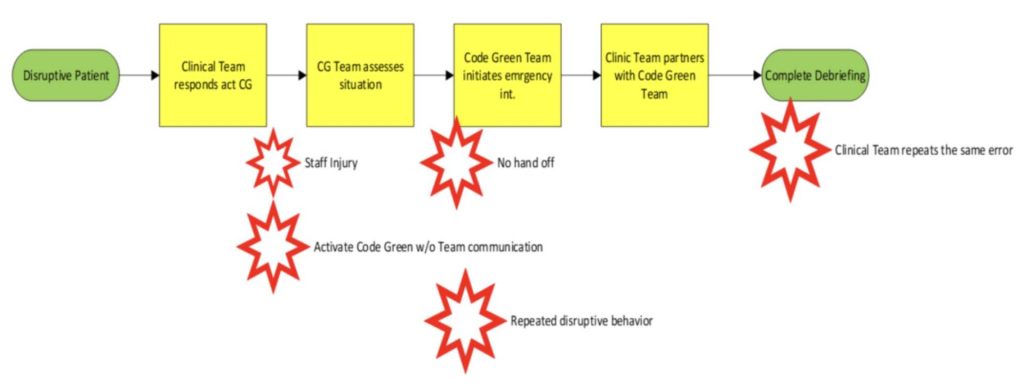
As the Project Facilitator, my goal was to create an environment where staff feel safe to address process failures and focus on the “why” of the situation and not the “who”. The current state map identified areas needing process flow improvement to promote safety during disruptive behaviors.
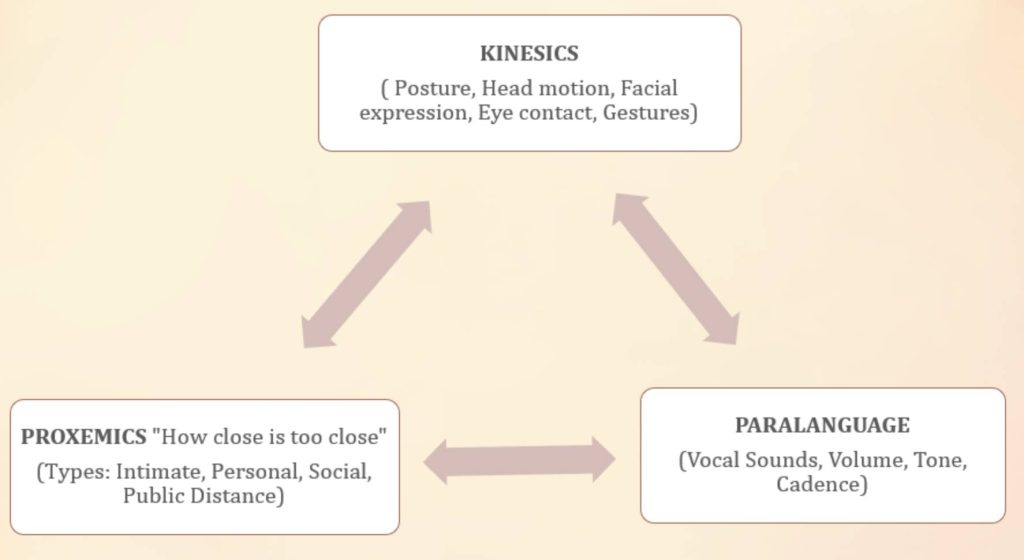
Kinesics, Proxemics, and Paralanguage were important key points utilized to address the process barriers when responding to disruptive behaviors.
Gap Analysis
The root causes were identified using the 5 Whys.
Solutions Approach
This phase was the most impactful and rewarding as the Lean Leader, placing the stakeholders first and supporting them in every step. The team focused on process improvement as a continuous journey, not on achieving an endpoint or one specific goal. From the project charter approval to the 8-month duration of the process improvement, I fostered servant leadership
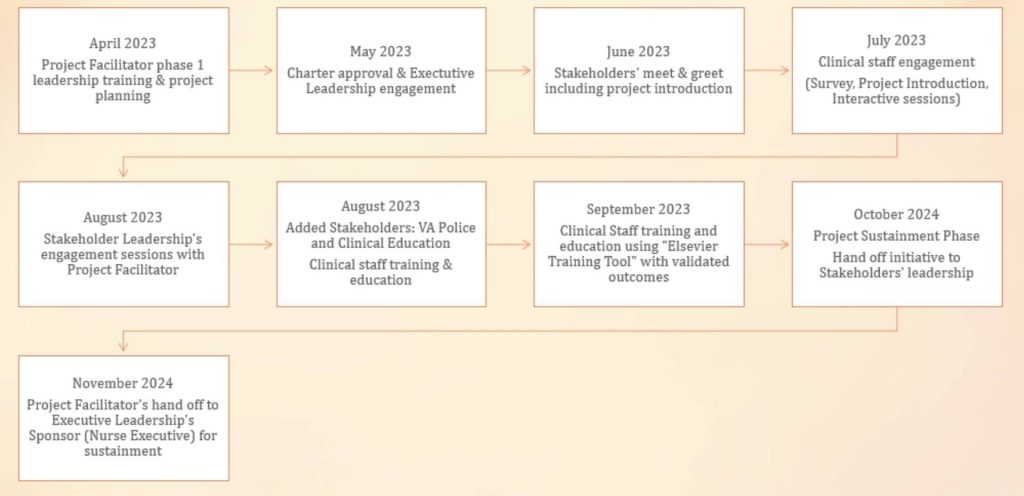
Figure 4: Process Improvement Flow of Partnerships
Looking at the solutions approach, there were 2 integral needs that stakeholders identified: (1) improve communication flow and, (2) establish a decision matrix to assist the clinical team to work collaboratively when a disruptive behavior is imminent or has occurred.
| Test of Change | Hypothesis | Root Cause | Impact | Effort |
| If we utilize a decision matrix in preventing and taking actions to disruptive behaviors. | We will expect effective communication flow when responding to disruptive behaviors promoting timely care to patients and safety among staff. | Lack of de-escalation skills using therapeutic communication and decision flow to activate effective management of disruptive behaviors. | High | Medium |
| If we use a communication tool to facilitate timely reporting of disruptive behaviors | we will provide timely patient care and decease the escalation of disruptive behaviors | Lack of de-escalation skills using therapeutic communication and decision flow to activate effective management of disruptive behaviors. | High | Medium |
Table 1: Solutions Approach
Rapid Experiments
During the team engagements sessions, I was privileged to share a Communication Tool that I have created and used with my varying leadership roles since 2012. It highlights the chronological steps of promoting effective communication in any type of clinical setting and leadership roles. It is a helpful tool in identifying where communication breakdown occurs, thereby allowing process improvement. From it being Timely and Specific (TS)- Appropriate, Respectful, and Collaborative (TS-ARC).
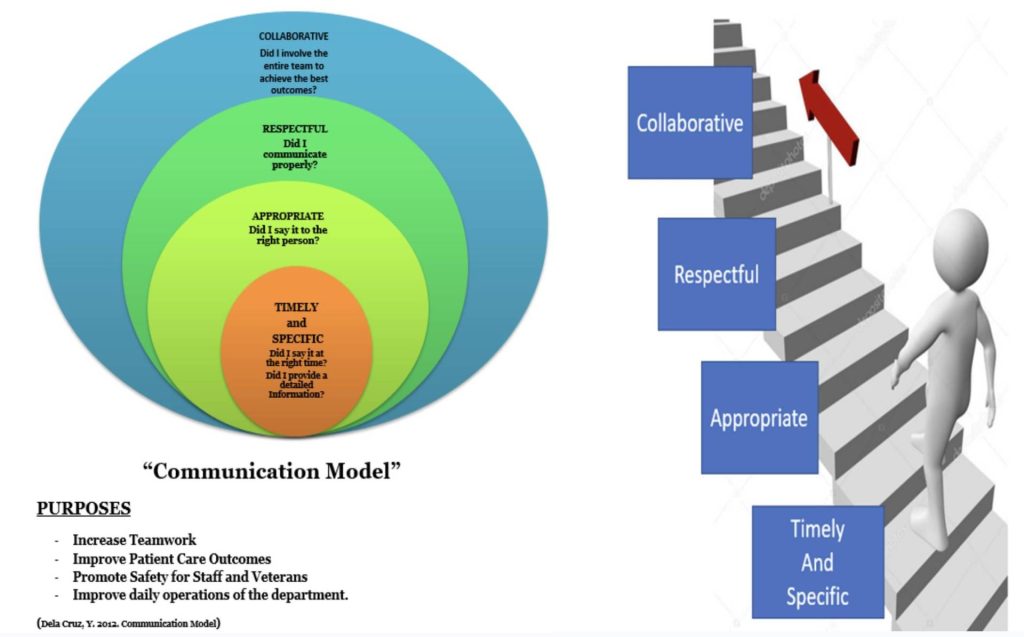
Figure 5: Communication Tool: “TS-ARC”
The communication tool was instrumental in addressing the barriers: (1) inability to deescalate disruptive behaviors (2) inadequate handoff between clinical staff (3) disengagement from clinical staff requiring the need for a decision matrix to support their team collaboration (4) lack of debriefing process. The engagement sessions of nursing leadership, clinical staff with representations from day and night shifts (N=180) provided a safe environment to address their learning needs. This included early partnerships for mental health consultations, working as a team to address imminent risks during disruptive behaviors utilizing the communication tool.
The next step was our development of a decision matrix to help establish appropriate level of care when disruptive behavior occurs. The decision flow promotes HRO principle addressing “sensitivity to operations” ensuring that systems and processes are established to promote safety.
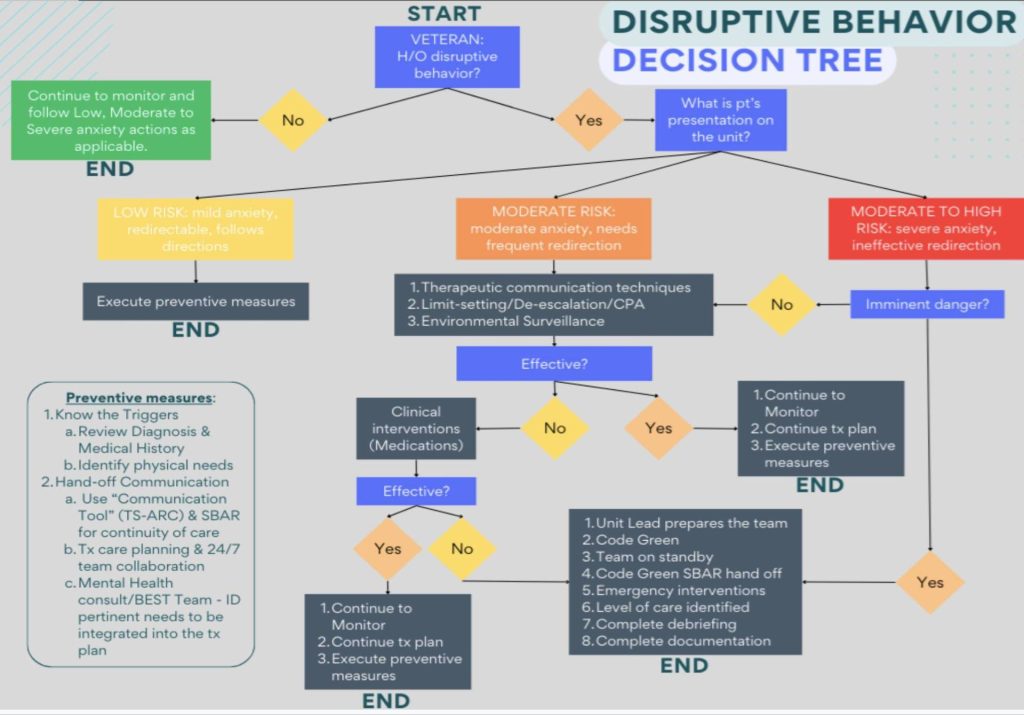
Figure 6: Disruptive Behavior Decision Tree
Confirmed State
The crisis communication initiative validated a “sense of belonging” to our front-line staff. They felt that their voices were heard in addressing safety issues including staff injuries, miscommunication, lack of teamwork, staff training and education. By Q1 of FY24, the initiative reached it sustained phase validated by reductions of staff injury, code green activations were limited to de-escalation phases, and emergent use of medications with positive patient outcomes. I partnered with our Nurse Executive to the hand off phase of this process improvement, giving her full support to extend the initiative to the CBOCs. The process map confirmed the effective flow resolving barriers.
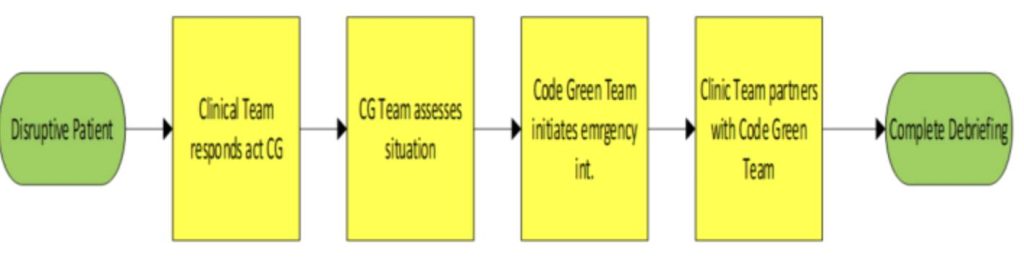
Figure 7: Process Map: Confirmed State
Insights
We celebrated our success, the stakeholders highlighted the strengths of their team work.
| What went well | What did not go well | Lessons Learned | Next steps |
| Team engagement. Learning & Applying Communication Tool Decision Matrix introduced promoted staff engagement. | Limited participation of one service stakeholder due to operational structure changes. | Staff engagement entails taking account of full representation. Impressive buy in from night shift staff. They felt a sense of belonging and have the voice to speak up and address their barriers when responding to disruptive behavior on off tours. | Extension of initiative to CBOCs. The next steps from this initiative include: (1) Simulation exercises as a safe learning space. (2) continued Skills Training and competency verifications (3) expansion of the initiative for other disciplines. |
Table 2: Insights
Summary
The HRO Value, Commitment to Zero Harm validated the sustainment of this initiative. The investment on staff training and competency supported avoidance of cost that could potentially require financial investment from staff injuries because of disruptive behaviors.
Workplace violence is costly and preventable, this initiative highly supported worksite analysis and hazard identification. It is a serious healthcare problem and contributes to employee dissatisfaction and burnout. As leaders, supporting a HRO entails our commitment; that safety and reliability is reflected in our vision, decisions, and actions. Second, promoting a culture of safety, values and practices should be utilized to prevent harm and learn from our mistakes. Finally, as this process improvement validated, continuous process improvement is a key component of safety.